Scientists use placental cells in lab to study virus
By Phillip Sitter | MU Bond Life Sciences Center
Scientists believe they have a better way to study how Zika virus can spread from a pregnant mother to her fetus — and their technique doesn’t even involve observations of babies in the womb or post-natal examinations.
“As soon as we heard about Zika, everybody’s light bulbs turned on,” said Megan Sheridan, a graduate student at the University of Missouri Bond Life Sciences Center.
Sheridan works in the lab of Toshihiko Ezashi at Bond LSC, and she, in turn, is part of a cross-campus team researching Zika with R. Michael Roberts, Alexander Franz, Danny Schust and Ezashi.
Roberts’ lab studies pluripotent stem cells — progenitor cells which can develop into any other type of cell in the body.
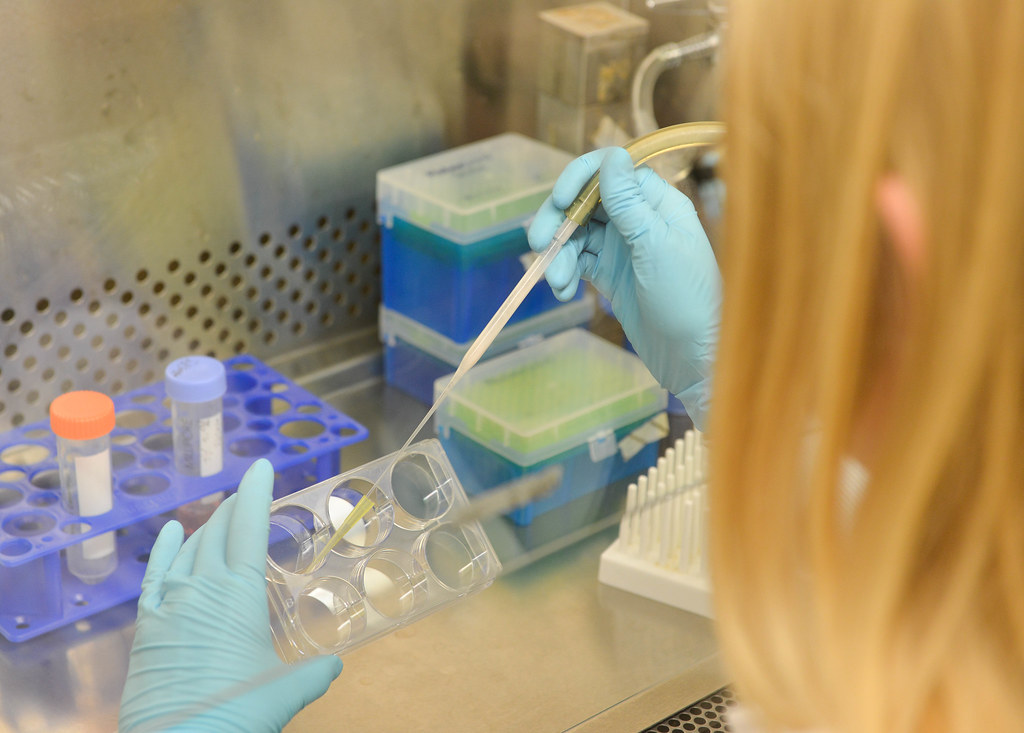
“We use the proper signals to drive stem cells to become like placental cells,” Sheridan explained. With this capability to stimulate stem cells with growth hormones and inhibitors at opportune moments, Roberts’ researchers realized they could create enough placental cells to create an environment similar to that of a womb in very early stages of pregnancy.
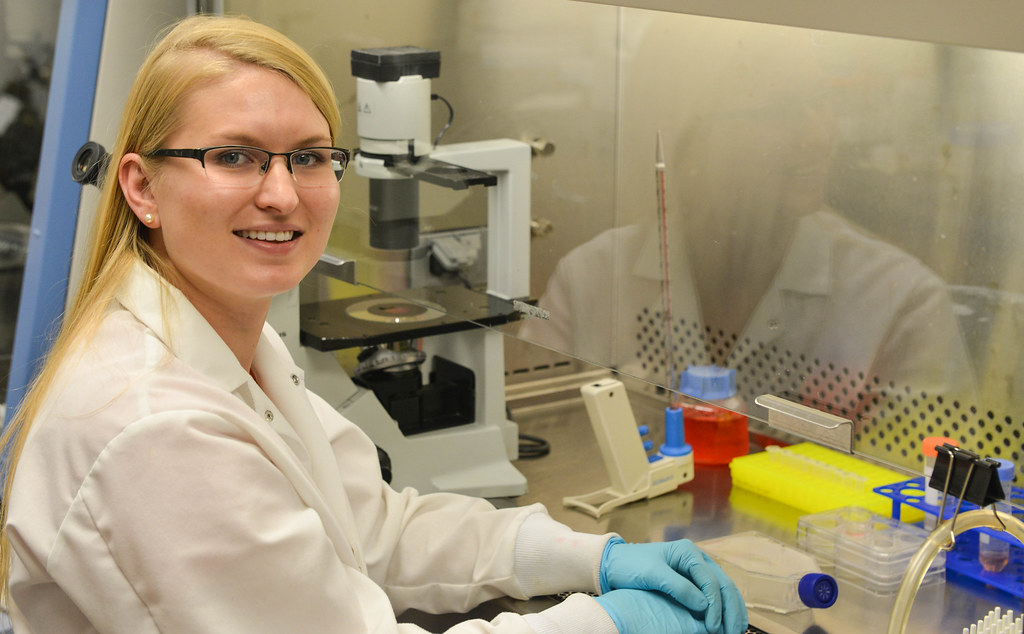
This is something which Sheridan thinks hasn’t been done before in regards to studying placental interaction with Zika. Their technique could give a look into the first trimester, when epidemiological studies say a fetus is most susceptible to infection.
Roberts’ lab is trying to understand the placental barrier’s vulnerability to Zika virus in its early stage of pregnancy. During this time, an infection could occur even before the mother is aware she is pregnant.
If the lab uses their technique to understand how Zika virus enters placental cells, then potentially they could also learn how to strengthen the placenta as a barrier to Zika and make it a first line of defense against infection of the fetus in the womb. If developing babies don’t get infected with Zika, then they won’t suffer the consequences of birth defects.
One such defect is microcephaly where a baby is born with a smaller than expected head, which may in turn be a sign that their brain has not fully developed. While infection with Zika virus is rarely fatal or otherwise severe in itself — many people don’t even develop symptoms — birth defects like microcephaly could cause further developmental problems like delays in learning how to speak and walk, intellectual disabilities, difficulty swallowing and problems with hearing and vision, according to global health organizations.
Microcephaly only became a widely documented effect of Zika after a particular strain surged across South and Central America with the infected mosquitoes that carry it, Sheridan explained, but this may be in part because previous Zika infections and outbreaks were themselves poorly documented.
While birth defects caused by Zika have drawn much media attention as the disease has spread northward through our hemisphere from Brazil, studies focusing on infection in the womb have only used placental material that has come to term. This may not be the most accurate way to see how the placenta gets infected in the first place early in pregnancy.
The pathway of Zika virus infection in lab mice isn’t really comparable to human infection, because mice aren’t infected with this virus naturally. Only lab mice that have had their genomes altered to be able to acquire the virus have susceptibility to the infection that can be modeled.
Roberts’ lab is currently working with the African strain of Zika and obtained strains from Southeast Asia and Central America recently. There’s about a 99 percent genetic similarity across strains, Sheridan said.
Zika virus was first discovered in Africa in Uganda in 1947, according to the Centers for Disease Control and Prevention. The first human case was documented in 1952, and subsequent outbreaks also occurred in Southeast Asia and the Pacific Islands. The Pan American Health Organization issued an alert about the confirmed arrival of the virus in Brazil in May 2015.
The lab has completed Zika infections of some of their stem cell-produced placental cells. Sheridan reassured that even though the lab works with live viruses, Zika is not airborne, and none of their work involves mosquitoes.
Roberts’ lab submitted one grant application earlier this year to the National Institutes of Health for funding for their research. While that application was denied, Sheridan said that they have a lot more preliminary data now and are hoping to submit a revised grant soon.
She said that their original work was “highly scored, but the funding level is still low,” meaning that obtaining funds for research into Zika virus is highly competitive nationally.
Legislation to fund more efforts into studying and preventing transmission of Zika virus is caught in congressional gridlock, according to The New York Times and other media outlets.
In the mean time, as the Roberts lab prepares its next grant application submission, Sheridan said of her efforts that she is “working hard to make progress on the project as quickly as possible.”
Please visit the CDC’s dedicated page for more information on Zika virus — including advice for travellers and pregnant women, description of symptoms and treatment, steps you can take to control mosquitoes and prevent other means of transmission of the virus and more background on the history and effects of the disease.

