Zooming in on the tools: TS33 Secretion System

Salmonella is one bacterium everyone’s heard of. It’s the scourge of meatpacking plants and involved in spinach recalls every year, causing unwelcome intestinal unrest and dangerous disease when encountered in high enough numbers.
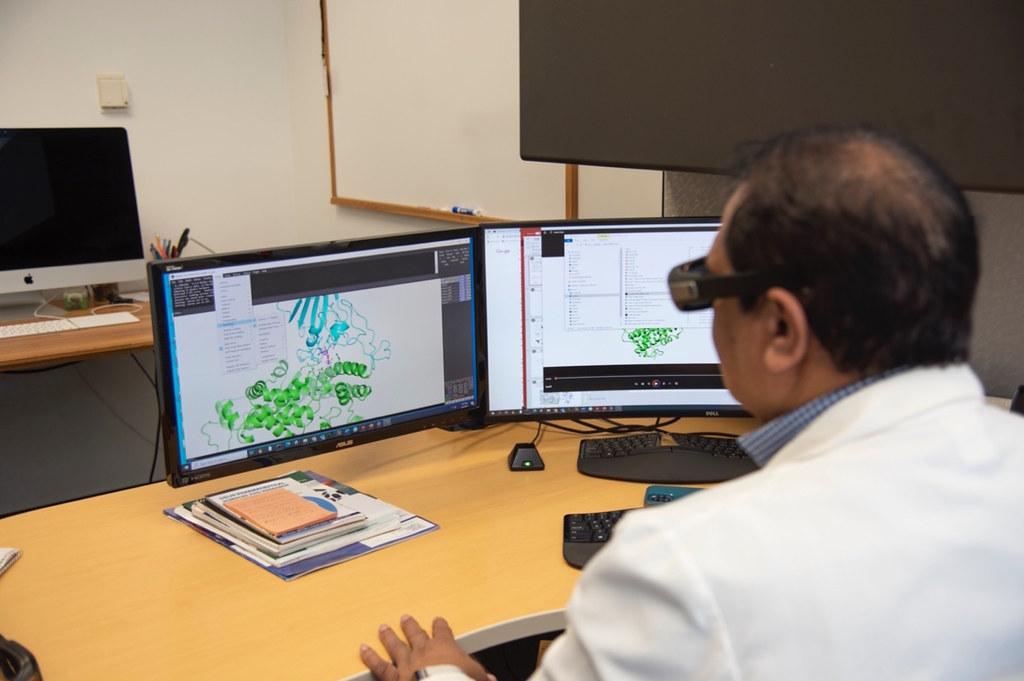
William Picking wants to better understand how to combat this and other food and water system hazards. The Bond Life Sciences Center scientist reached down to take a piece of paper to quickly jot down a drawing of a nifty way some bacteria have evolved to avoid the defenses of the animal cells it infects. One of the focuses of his research is to determine how the bacterial type 3 secretion works. Understanding this secretion apparatus may help scientists create better, more targeted drugs to fight pesky bacterial infections and outbreaks.
His drawing showed the type 3 secretion apparatus (T3SS), the bacterial structure that injects specialized proteins into cells to avoid being detected and attacked by those cells. In some cases, the apparatus actually invades those cells so the bacteria can grow inside them. Scientists like Picking aim to use proteins from this needle-like structure to develop new strategies to prevent disease
This “injectosome” is basically a syringe. Composed of a base with a channel through it connected to a needle, this apparatus injects into and through the membrane of its host cell to get its proteins inside.
Scientists have a general idea of what the T3SS secretion apparatus looks like, but Picking’s current research focuses on understanding exactly how the injectosome works as a microscopic machine at a deeper level.
Picking and his team zoom in on the specific way that it selects the proteins to be secreted and energizes that process so they can deliver their specialized proteins.
This process must be coordinated so that the proteins are properly injected into the cell, so they invade those cells or, in some cases, kill the host cells trying to harm the bacteria.
The power behind this process comes from the ability of bacteria to recognize the surface of the organism to form a hole in the host cell membrane. The needle then passes those proteins through the hole.
The parts of the injectosome that are inside the bacteria are involved in determining what proteins are secreted and in what order. This overall internal segment is called the sorting platform and it also provides the actual power that drives the secretion process, causing the secreted protein to be unfolded and then forcing it through the needle and ultimately into the host cell. It makes the injection of this process easier and speeds it up.
“We have a general idea of what the sorting platform looks like but our research focuses on improving our understanding of this structure to get at the mechanisms guiding secretion,” Picking said. “We even want to understand the movements within this structure that are part of the secretion process. “
Picking’s main focuses are bacteria like Salmonella and Shigella, but other bacteria like Pseudomonas aeruginosa can shut down the communication some immune system cells use to combat an attacking microbe.
“By understanding this apparatus at a high resolution, at a detailed structural level, we can potentially design drugs to inhibit the process of infection.” Picking said.
The trick is to reverse engineer a drug that operates like an antibiotic from the knowledge of T33s. That small drug could block the process of infection, and the body’s immune system can kill off the invader.
The problem that arises for scientists is the antibiotic often kills the bacteria. This leads to antibiotic resistance, a process called selective pressure. That’s not good news. The drug engineered from reverse T33s shuts off the bacteria instead of killing it. But, by shutting off the bacteria, your immune system will naturally recognize the pathogen or foreign invader and then destroy it itself. This is an ingenious idea, gaining popularity with bacterial scientists meant to avoid the often-inevitable bacterial resistance.
Bacterial resistance is a chronic problem in our world where antibiotics become less effective as the bacteria evolve around its protection. This causes problems the problems you hear in hospital systems where MRSA bacteria threaten life after antibiotics fail to fight them off or even how low levels of antibacterial agents in hand soap create more persistent colonies on surfaces.
Zooming in on the T3SS injectosome may give clues to better fight infection and reduce the number of people affected by dysentery and other common bacterial infections.
“It’s a great goal, not a goal our laboratory will accomplish in the immediate future, but we hope to provide the information for someone else to create these drugs to get around the problems of antibiotic resistance.” Picking said.