Lorson lab publishes research on a new therapeutic path to help treat spinal muscular atrophy
By Phillip Sitter | Bond LSC
Imagine you are forced to jump out of an airplane.
Luckily, you find a parachute that even has a backup chute. You leap out of the plane and free-fall.
You pull the cord to open your parachute, but it doesn’t open. Don’t panic, though, you have a backup. But, you pull that cord and nothing happens. Now you face the reality of a death as firm and un-yielding as the ground rushing into your view.
This air disaster mirrors the mechanism and mortal threat posed for people born with the genetic problem that causes spinal muscular atrophy (SMA).
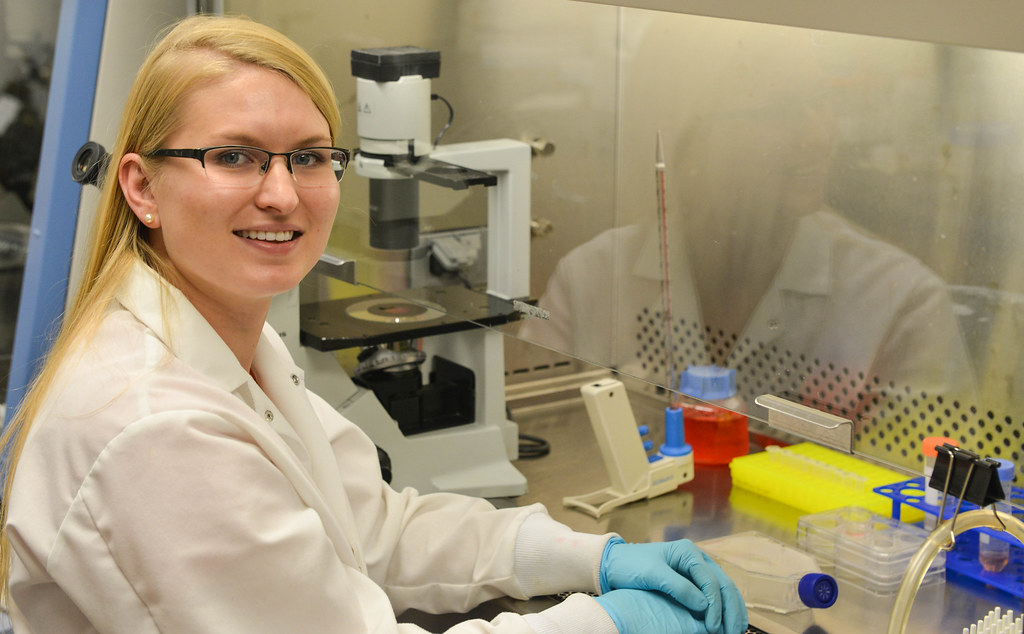
Chris Lorson’s lab at the Bond Life Sciences Center would like to change that situation by making an effective genetic backup to the defective gene that results in SMA. The journal Molecular Therapy, a publication of Nature, recently accepted their findings for publication.
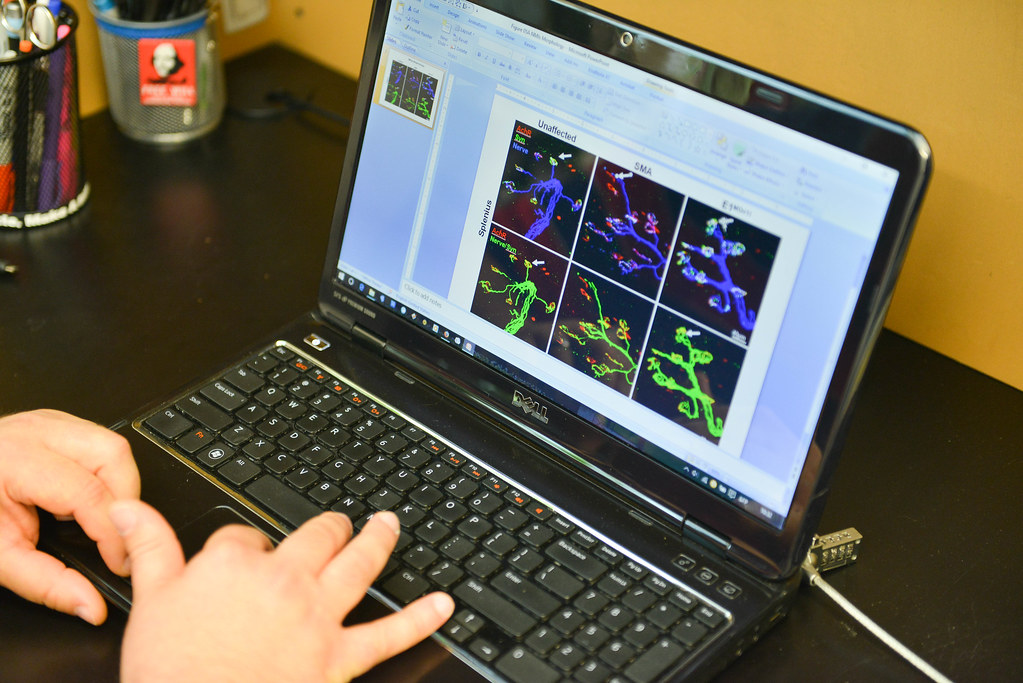
The defect occurs in a specific gene called Survival Motor Neuron (SMN). If the SMN gene is defective because of mutation, this causes a deficiency of the SMN protein it is supposed to produce. Without this protein, the neurons that control muscle movement malfunction. Signals cease to stimulate muscles.
Muscles that are not stimulated atrophy, grow weak and waste away. At first this happens with the skeletal muscles, which leads to loss of motor function for simple activities like walking and swallowing. If it happens with the muscles that control breathing, you die.
News of the disease often presents a devastating prognosis. Infants have it worst; babies diagnosed with SMA only have a life expectancy of two to five years from birth.
Fortunately, our bodies have a sort of backup for the SMN gene, another one called SMN-2. But, like a useless backup parachute for an unlucky skydiver, SMN-2 isn’t actually very good at producing proteins of the quality needed to stave off SMA. It might just be a vestigial trait on its way down the evolutionary drain — it doesn’t even exist in the closest primate relatives of humans.
Discoveries in the Lorson lab look to make the SMN-2 gene an effective backup, and their recent publications indicate that this may be a viable possibility for future SMA treatments.
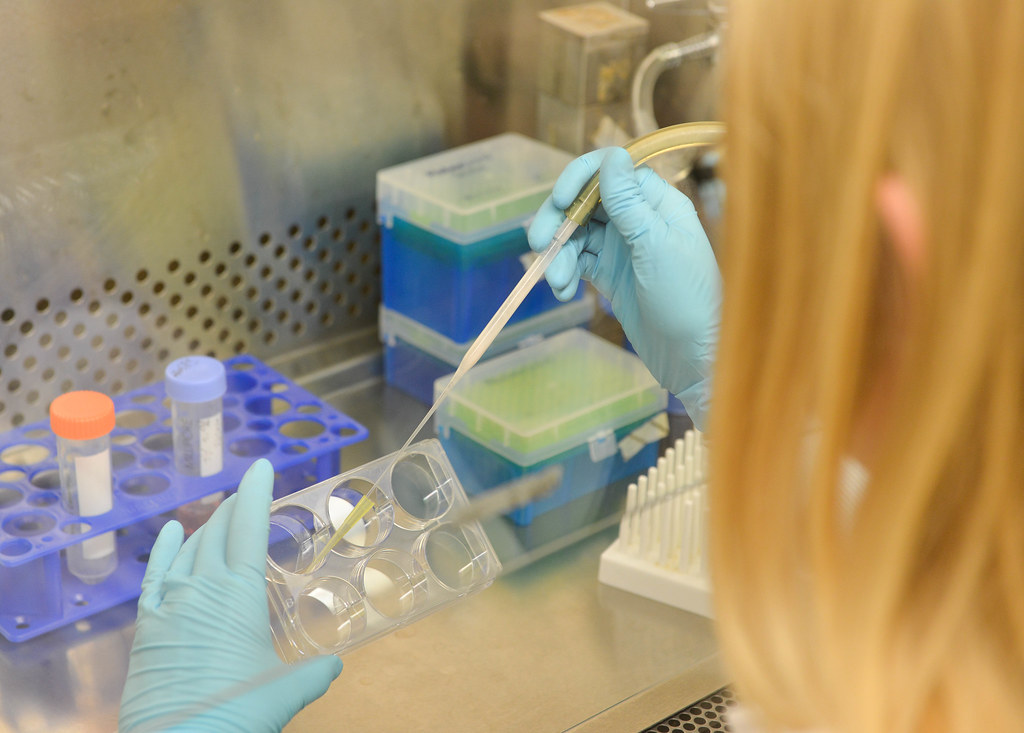
“What we’ve been working on in the lab is a potential therapeutic, and what it does, it’s a large small molecule that is called an antisense oligonucleotide, or ASO,” Lorson said. “And this is something that is essentially a synthetic piece of nucleic acid that is able to go in and bind to a specific sequence within a gene.”
Once bound to SMN-2, the ASO is designed to alter mRNA splicing, “essentially, the editing of a gene,” Lorson said. Speaking in terms akin to products leaving a factory, Lorson said that the attached ASO makes SMN-2 produce good quality proteins, the ones that it wasn’t able to produce before.
In other words, suddenly the backup protein-factory that was making poor-quality products is now pumping out top-of-the-line stuff that will work.
Previous research identified a strong ASO contender to experiment with, and Lorson said current research is about optimizing an ASO to extend survival times in mice with SMA — from just 13 days to five months after only one injection at birth.
Lorson stressed that his lab’s achievement doesn’t promise a fast cure for SMA. He said it is unlikely a single compound will address the full gambit of effects that people with SMA suffer, especially given that people can be identified as having SMA at any time from birth through later in life — often late onset SMA tends to be less severe than diagnosis as an infant.
There’s not yet any single compound treatment for SMA that has been approved by the Food and Drug Administration, Lorson said, so he cautions against getting hopes up of for a revolutionary treatment for SMA coming onto the market soon — “Near future but not tomorrow.”
He acknowledged, though, that “from a research perspective, things seem to be moving at lightning speed, but if you are a patient or a family member, things can never go fast enough, so I think there’s a realized sense of urgency, whether or not it’s for patients who don’t have the disease yet, are not born, or for patients who have had the disease for a decade and are wondering when their opportunity would come.”
Lorson’s work is funded in part by Cure SMA, FightSMA and the Gwendolyn Strong foundations. Erkan Osman, a post-doctoral fellow in Lorson’s lab and the first author on the most recent paper, won the emerging investigator award from FightSMA and Gwendolyn Strong in 2015.