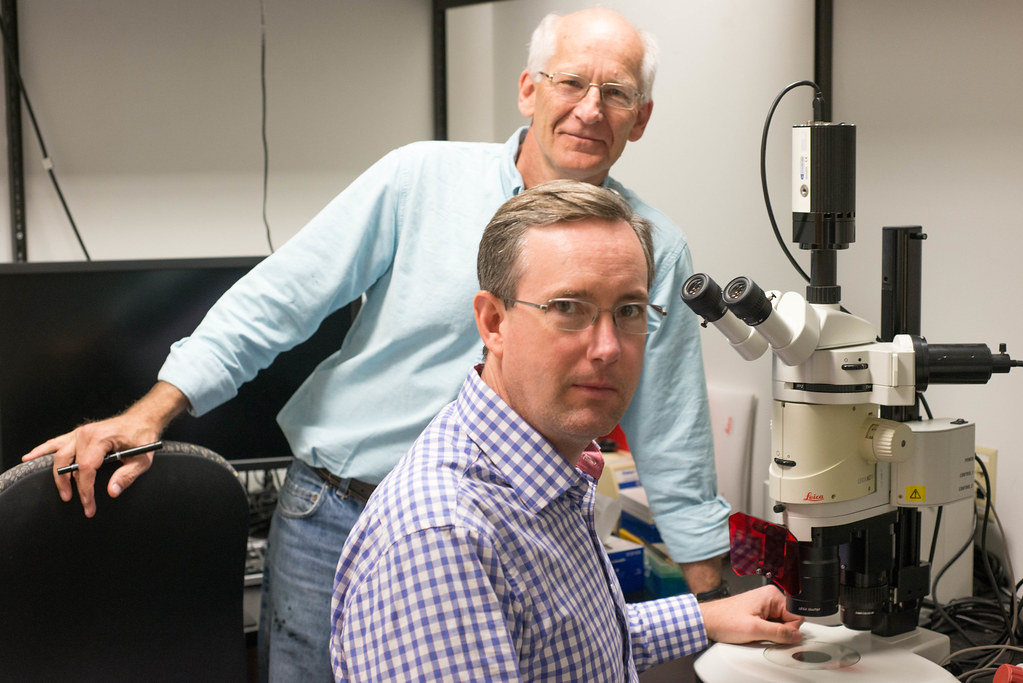
Chris Lorson, a professor of veterinary pathobiology, and Mark Hannink, a professor of biochemistry, want to find a new way to help motor neurons live a long and healthy life. Their question: what’s the relationship between motor neuron sruvival and a cellular component called mitochondria?
The two researchers at the Bond Life Sciences Center were awarded preliminary funding from the Bond LSC to pursue this question. Their findings could lead to new targets for therapies to treat a type of muscular dystrophy called spinal muscular atrophy, or SMA.
Spinal muscular atrophy, a genetic disease characterized by the death of motor neurons in the spinal cord, is caused by a mutation in the Survival Motor Neuron 1, or SMN1, gene. Patients with SMA develop muscle weakness and deterioration that spread inwards from the hands and feet, which progresses to interfere with mobility and breathing. The severity of symptoms and time of onset depend on how well a related gene is able to compensate for the lack of SMN1. As a result, treatment strategies usually focus on improving the activation of SMN1’s back-up gene.
Hannink and Lorson, however, are interested in a different pathway that is related to mitochondria dsyfunction.
Mitochondria are like the cell’s battery packs. Produced in the cell body, mitochondria migrate to the other end of the motor neuron to provide the energy to send electrochemical signals to recipient muscles and nerves. When mitochondria break down, the cell packs them into vacuoles that return to the cell body for recycling or removal.
“I saw a report that said that in SMA, there’s evidence for dysfunctional mitochondria in spinal motor neuron atrophy,” Hannink said. “My lab knows something about how mitochondria respond to stress.”
“There’s a lot of information out there that hints at it,” Lorson, an expert in SMA, said. “A number of the same responses you see in the stress pathway are also activated in neurodegeneration.”
To test their hypothesis, Hannink and Lorson plan to make motor neurons from pluripotent stem cells taken from people with and without SMA, and compare mitochondrial function and cell survival between the two groups. Then, they will test if a number of different genes that are known to be important for mitochondrial function will affect motor neuron health in both SMA and non-SMA derived cells.
“If you look at the tool chest of SMA therapeutics right now,” Lorson said, “you have a number of very obvious targets.”
Most approaches aim to boost the performance of the SMN or its back-up gene, but there are also options like neuroprotectants and skeletal muscle activators. Molecules that maintain healthy mitochondrial function could be another possibility.
“These are things that don’t worry about the state of the SMN gene and are targeting something in addition to, supplemental to or as an alternative to SMN,” Lorson said. “And that’s where this project would fall.”
This seed funding is one of seven awarded this year at the Bond Life Sciences Center. These awards, which range from $40,000 to $100,000 in funding, foster inter-laboratory collaboration and make possible the development of pilot projects.

