Researchers find evidence of a genetic modifier that can improve symptoms of Spinal Muscular Atrophy
Eleanor Hasenbeck | Bond Life Sciences Center
Two new potential treatments might improve the lives of patients living with Spinal Muscular Atrophy.
Researchers in the Lorson lab at Bond Life Sciences Center recently produced a new drug that increases the lifespans of mice with SMA, and they found evidence that an increased level of the protein plastin 3 lengthened life span and improved the animal’s nerve function.
Two genes impact Spinal Muscular Atrophy, SMN1 and SMN2. In a healthy body, SMN1 creates a protein called SMN that helps maintain motor neurons controlling muscle movement. If someone is born without SMN1, their body relies on SMN2 to produce this protein, but a small change in the SMN2 gene causes it to make much less of the protein than needed. This leads to SMA, a disorder where an individual loses motor and nervous function, often starting in childhood, over a number of years.
Although rare, sometimes siblings develop SMA, providing an unusual insight into SMA development. Discordant siblings — or siblings that both have SMA but have different severities of the disorder— suggest that other factors could contribute to SMA.
Researchers are investigating why this happens. One theory is that a “genetic modifier,” another gene or protein elsewhere in the DNA, impacts the severity of SMA. The protein plastin 3 could be this modifier.
Plastin 3 doesn’t improve the severe SMA mice, but extended the lives of mice with more mild cases of the disorder. The Lorson lab created its own SMA drug, an antisense oligonucleotide that allows SMN2 to produce a functional protein. The drug is capable of extending survival of SMA mice from approximately 13 days up to 150 days from a single treatment. The typical lifespan of a lab mouse is 1.3 to 3 years.
Kevin Kaifer, a graduate student in the Lorson lab, gave the SMA mice a low dose injection of the drug, increasing their lifespan to about 30 days. Then, they modified a gene in the mice to increase the level of plastin 3. Mice that received the drug and the plastin 3 therapy lived about 40% longer than mice that received only the drug.
Lorson said the results provide proof of concept that plastin 3 does not make more SMN, but actually decreased disease severity. The SMA mice showed improved neuromuscular junctions, the sites where nerve cells fire electrical impulses to the muscles in the body.
“That’s really where plastin 3 is designed to function, at the neuromuscular junction,” Lorson said. “So that brings the idea of plastin 3 full circle; it does not increase SMN, but it does improve the function of the nerve which is where plastin 3 is supposed to function normally.”
This discovery shows promise for a future treatment to some with the disease.
“SMA is a very broad clinical spectrum disease, so there are patients who have an incredibly severe form, and patients that don’t develop disease until adulthood,” said Chris Lorson, a Bond LSC scientist. “Perhaps one therapy is not going to address that very broad clinical spectrum, and you’re going to need to address different parts of the disease with different therapeutics.”
Despite it’s relative rarity as a disease, new treatments for SMA are hitting the market. In December, the Food and Drug Administration approved Spinraza, an antisense oligonucleotide similar to the drug the Lorson lab. But the infrequency of SMA means treatment comes at a cost: $750,000 for the first year of Spinraza and $375,000 for subsequent years. Spinraza is an FDA-designated orphan drug, meaning it’s a treatment for a disease that affects less than 200,000 people in the U.S. To incentivize research into rare diseases, The Orphan Drug Act allows pharmaceutical companies longer exclusive patent rights. Drugs that treat rare diseases that impact children, including Spinraza, can be allowed priority review, basically putting these drugs on a faster track from lab to market. Though the act has led to more research in certain diseases, it has sparked controversy as patients with no other treatment options are burdened with the resulting drugs’ high cost.
Still, it’s the first FDA approved treatment available to the 9,000 Americans living with SMA.
“I think collectively this is a very exciting time in the SMA field, whether we’re talking about SMN targeting compounds or drugs that are capable of augmenting function,” Lorson said. “To have a rare disease that has so many shots on goals, so to speak is really exciting.”
“The SMA community is really a model for how foundations, families, patients and government agencies can come together,” Lorson said. He said families and government agencies are often in the same room as academics, biotechnology and pharmaceutical companies during meetings.
“The amount of support from the patients, the families and the non-profit world has really helped drive SMN research… I think that’s really helped push SMA from an unknown 20 years ago, to an approved drug.”
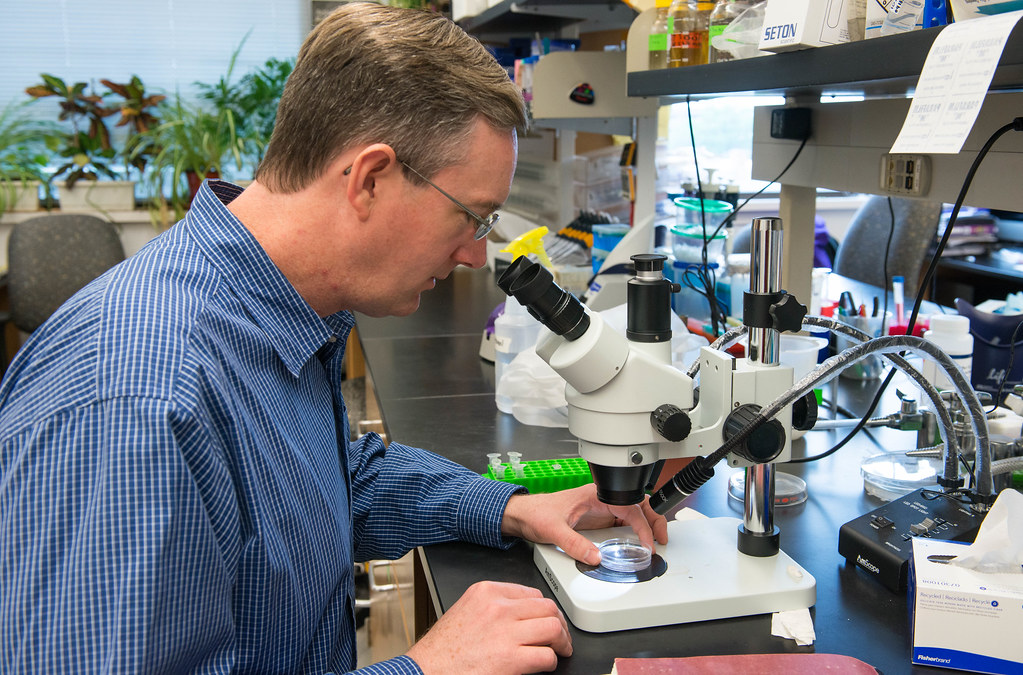
Christian Lorson is a professor of veterinary pathobiology at the Bond LSC. His research focuses on spinal muscular atrophy.
The results of this study were published in an article in JCI Insight, “Plastin-3 extends survival and reduces severity in mouse models of spinal muscular atrophy.” This work is partially funded by grants from the Muscular Dystrophy Association, FightSMA, the Gwendolyn Strong Foundation, and the Missouri Spinal Cord Injury/Disease Research Program. CureSMA provided the initial support for the development of the drug/antisense oligonucleotide used in these studies.