By Sarah Kiefer | Bond LSC
Some of the most fascinating things in science happen at the border where one organism interacts with its environment.
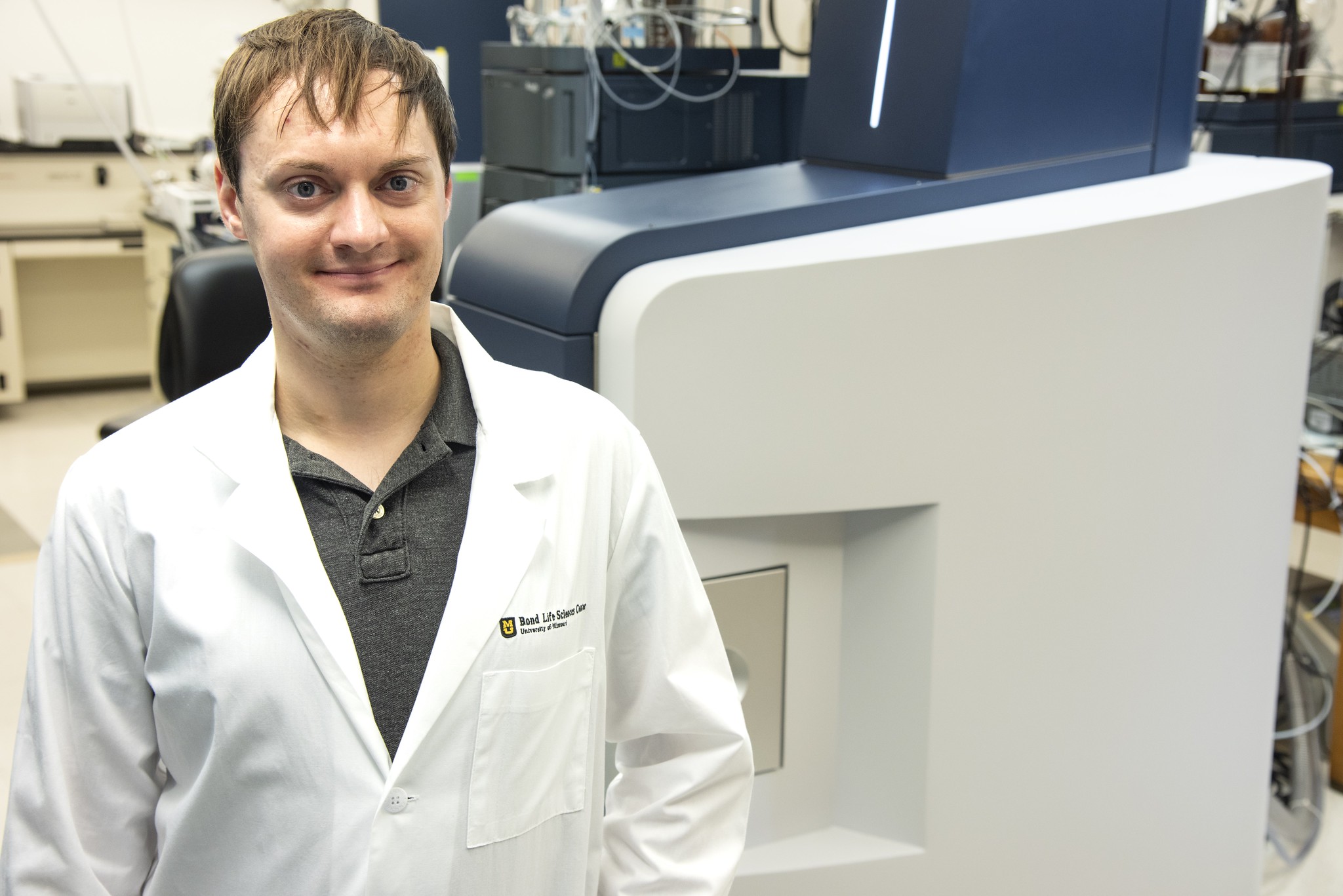
That’s the case with root border cells, and Clayton Kranawetter is one individual exploring this frontier.
Kranawetter recently received a $223,000, two-year USDA National Institutes of Food and Agriculture Postdoctoral Research fellowship for his project on this group of cells. This fellowship is a part of a larger $12 million investment in multiple institutions by the USDA to expand research in the area of agricultural microbiomes. The University of Missouri is among 17 research institutions to receive funding.
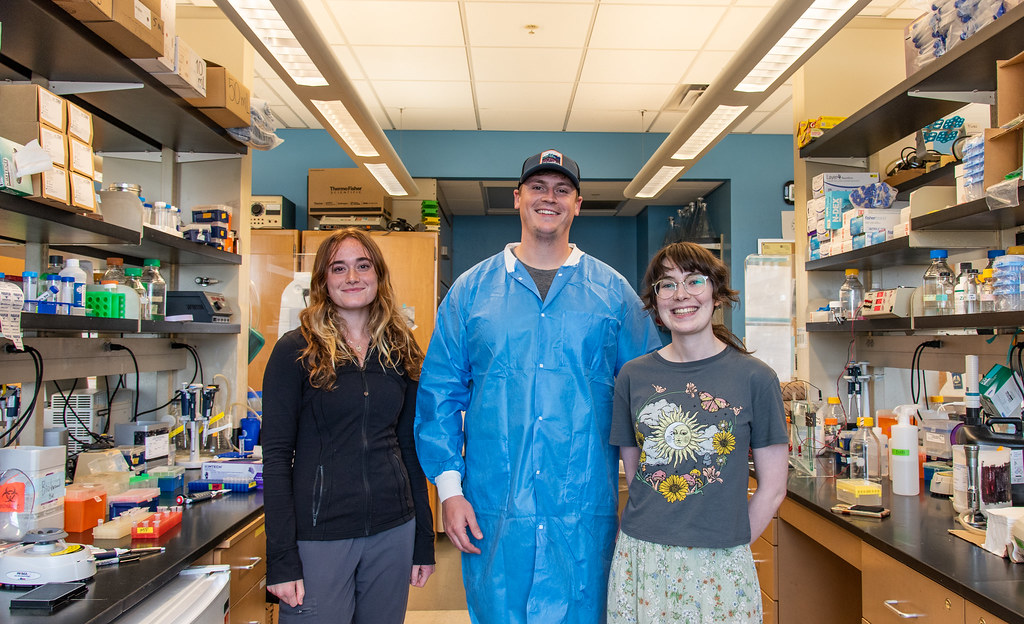
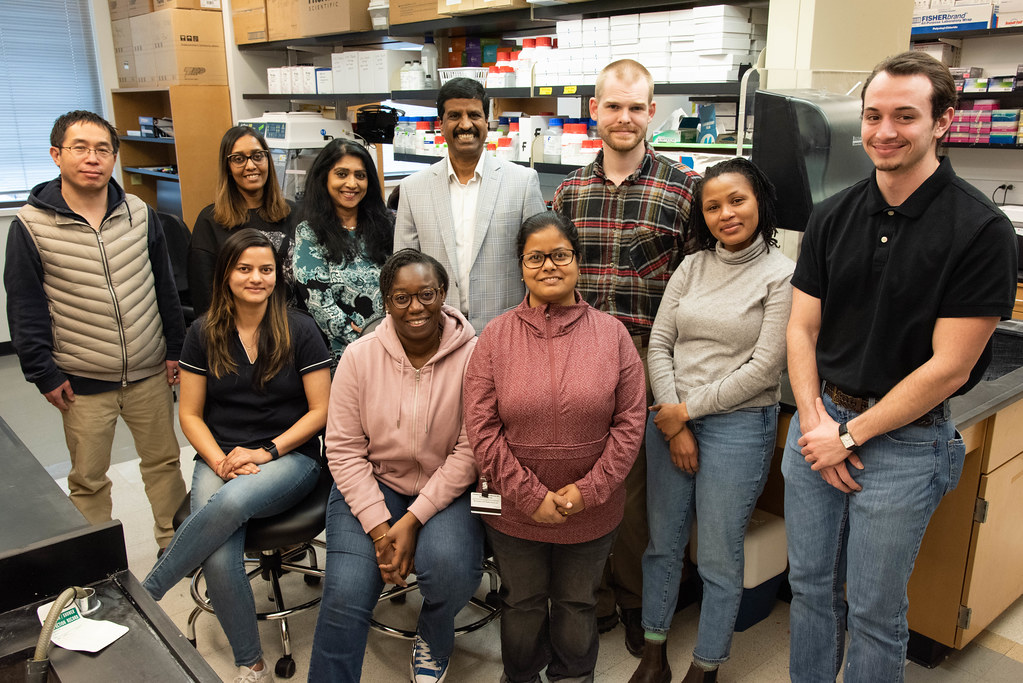
“I’m still shocked by receiving the award. I was already having a good day when I received my award notice. I found a good parking spot in the garage and a quarter on the sidewalk, but then I got the email” said the postdoctoral fellow in the Lloyd Sumner lab at Bond Life Sciences Center. “I thought it was a mistake at first and then I realized, ‘oh, this is real.’”
This fellowship will sustain his work in an influential way as he dives into the secreted metabolites and mechanisms of isolated border cells and their impact on rhizosphere dynamics.
Metabolites are small molecules made or used when a cell breaks down food, reacts to certain signals or completes other essential processes. Some metabolites, such as glucose, are part of an organism’s central or primary metabolism and its basic life functions. Other metabolites, such as secondary or specialized metabolites, are less essential to sustaining life but no less integral as they help with plant defense responses. Identifying these metabolites can help researchers predict how plants will react to various biotic and abiotic conditions, such as high light, stress from salt, symbiotic interactions, and defense against pathogens.
“I love science because everything is a puzzle,” Kranawetter said. “Sometimes the puzzle is a struggle to put together and can look quite different from what you expected, but after everything is complete, it is always rewarding and empowering to see how the pieces fit together.”
Kranawetter’s work focuses on root border cells, which are vital to plant root health. These cells arise from the root epidermis, where the cell wall breaks down and the cells are physically released from the root but still surround the root tips. Border cells are held in place through a water-soluble, complex secreted matrix consisting of a polysaccharide mucilage, comprised of DNA, proteins, and metabolites. As their encasing material is water soluble, upon contact with water they wash away but are rapidly replaced within 24 hours after their removal. After border cells separate from the root tip, Kranawetter conducts large scale genetic reprogramming to divert most of their resources to secretion and specialized metabolism. In doing so, they serve a protective role against infection and environmental stress, but the scope of their functions is far from fully explored.
“Border cells are still very niche, and we don’t fully understand how they’re contributing yet, but we’re starting to see that they are more major players in the rhizosphere than we thought initially,” Kranawetter said.
Root border cells appear across most plant species. They are known influencers of dynamics within the rhizosphere — the layer of soil that is in direct contact with root secretions — but there are still a large number of unknowns about them.
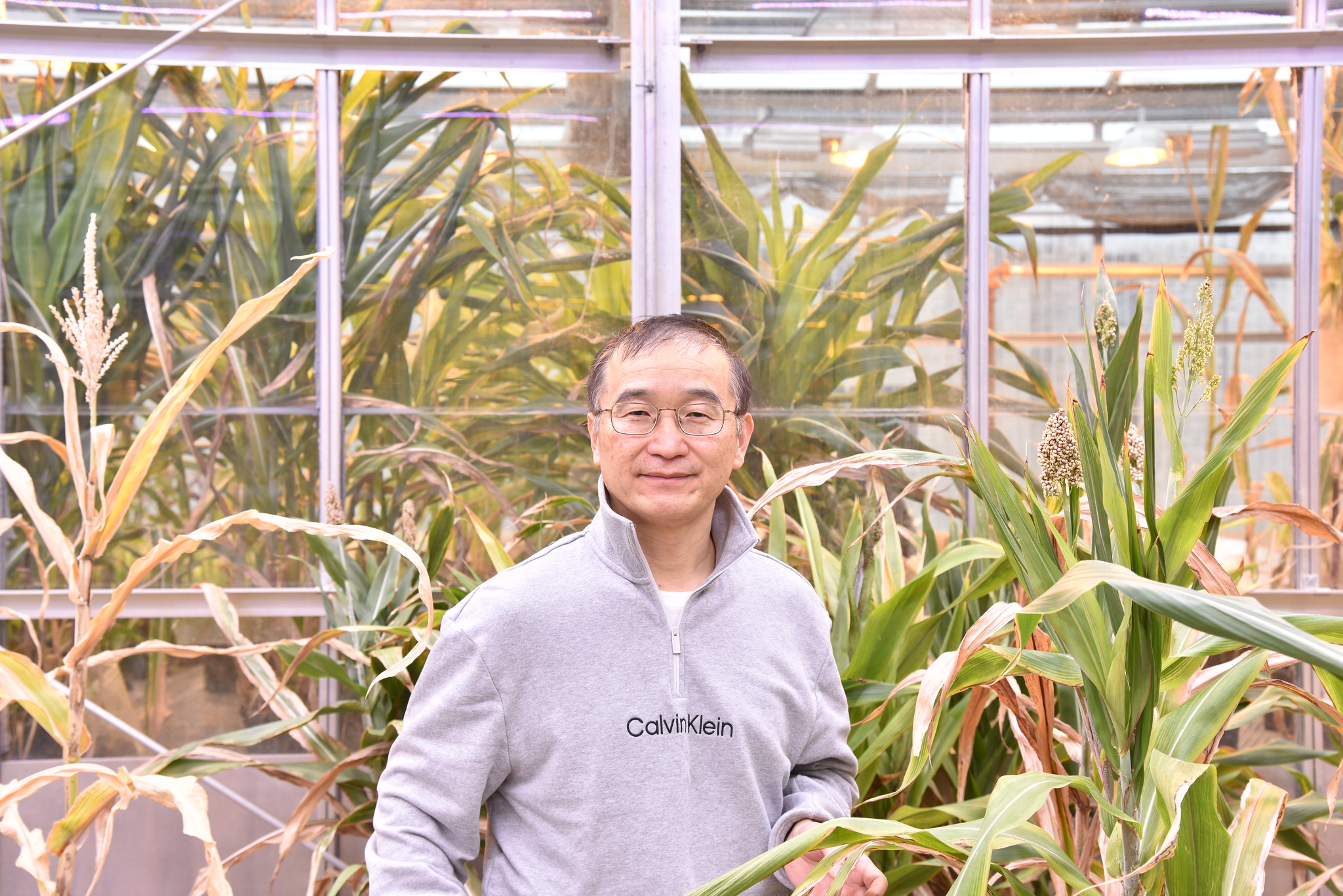
Kranawetter’s previous work dealt with metabolites, or small molecules, and their differential accumulation in root tissues. He collected root border cells and separated individual root tissue types to create a metabolite atlas based on the Arabidopsis eFP browser – a computer program that shows the relative intensity of metabolites by tissue type in a heatmap context. This project builds on his work to further identify the molecules border cells secrete and how they mediate plant-microbe interactions.
Although this project does not directly correlate with his current research in the Sumner lab focused on differential metabolite accumulation in cultivated elderberry plants, it will allow Kranawetter to stay in plant tissue research, build on the foundational mass spectrometry knowledge he accumulated during his Ph.D. and incorporate microbiological techniques to border cells.
“Working on elderberry plants was a good chance for me to start a different project in a distinct plant system, which has been nice,” he said. “And this fellowship will be a great opportunity to apply my current research skills and knowledge base while also developing new abilities.”
For the NIFA fellowship, Kranawetter generated a project narrative, abstract, budget, a logic model, references, and a data management plan, among many other materials. He also utilized a three-member administrative board to support and look over the project in order to assist and give feedback each step of the way.
“This will be a project for me to get out of my comfort zone and gain new expertise compared to what I have done in the lab previously,” Kranawetter said. “It’s nice to have a different perspective when, instead of having a bunch of giant elderberry bushes in the greenhouse, I’m working with three-day-old seedlings.”
The fellowship allots Kranawetter the resources and time he needs to monitor border cell metabolite secretions and their methods of secretion. Kranawetter also observes the bioactivities within an organism living in symbiosis with its pathogens, the microorganisms that cause disease.
“The field of mass spectrometry allows me to apply novel technologies and software systems, while plant sciences allow me to explore the vast diversity of compounds that plants naturally produce,” Kranawetter said.
Kranawetter applies what he knows about border cells in experiments on Medicago truncatula — a close relative to alfalfa — and observes how border cells use their secretions to affect the rhizosphere.
“The question we’re aiming to answer is how are these secretions going into the environment and what role are they playing,” Kranawetter said. “I wanted to get back to my roots with this because as a mostly technical lab, I haven’t done a lot of molecular biology in some instances.”
Kranawetter first removes the seed coat from M. truncatula and sterilizes them in order to protect them from bacterial or fungi contaminants. Next, he places the seeds on a petri dish containing water agar overlaid with sterile filter paper so that the roots remain on top, as opposed to normal methods of plating directly on top of the agar. This ensures that the roots do not penetrate the agar, where border cells would be lost. Although some cells are still lost due to the minimal contact with the filter paper, most remain for later harvest. The final step is to dip the roots in water and harvest border cells — ones that freely come away from their root system — for closer investigation.
As part of his fellowship, Kranawetter is probing for transcripts and proteins associated with metabolite secretion. His results will help determine how border cells affect their environment through their secretions. Kranawetter’s interest in this field stems from his love of plants and technology, both of which he uses in his daily lab work.
“One of the major benefits of being in the Sumner lab is that we’re getting to use very sophisticated instrumentation and applying it to something that we probably would not have been able to examine otherwise,” Kranawetter said.
Kranawetter’s fellowship lasts 2 years, so he hopes this exploration expands our understanding of border cell interactions with the rhizosphere.
“I love this type of research because I get to do a lot of different things! I grow plants, work at the bench, and also use cutting edge instrumentation,” Kranawetter said. “Being able to work in such a diverse manner makes me feel empowered as a scientist.”
Find details on Kranawetter’s fellowship at the USDA NIFA website.
The U.S. Department of Agriculture’s National Institute of Food and Agriculture (NIFA) announced an investment of $12 Million to Advance Research in Agricultural Microbiomes. Microbiome research is critical for improving agricultural productivity, sustainability of agricultural ecosystems, safety of the food supply, carbon sequestration in agricultural systems, and meeting the challenge of feeding a rapidly growing world population. Research supported by the Agricultural Microbiomes in Plant Systems and Natural Resources program area priority within the Agriculture and Food Research Initiative (AFRI) will help fill major knowledge gaps in characterizing agricultural microbiomes and microbiome functions across agricultural production systems, and natural resources through crosscutting projects. AFRI is the nation’s flagship competitive grants program for food and agricultural sciences.