
By Sarah Kiefer
The spikes that protrude from SARS-CoV-2 present a topography of peaks that drive one MU researcher to ask more questions.
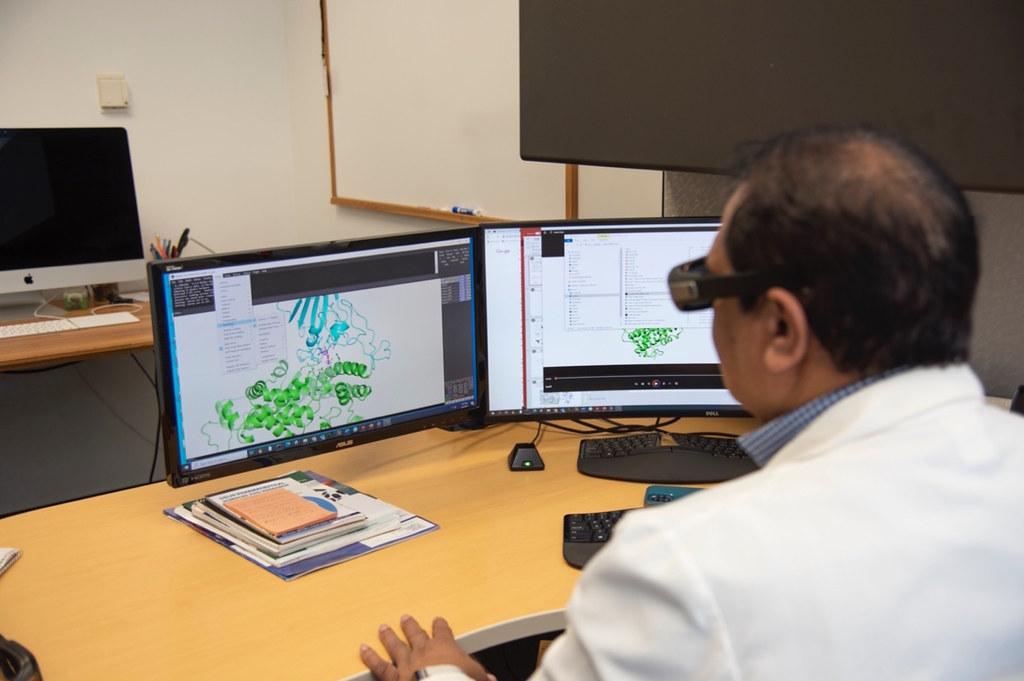
To Kamal Singh, a principal investigator at Bond Life Sciences Center, assistant professor in the MU College of Veterinary Medicine, and the director of the Molecular Interactions Core those spikes are a changing map with every new variant of coronavirus, and they lead his lab to study its constant evolution of mutations and proteins.
The Singh lab recently found an unexpectedly high number of APOBEC-mediated mutations among a patient cohort from South India, who were vaccinated and have taken remdesivir to treat COVID-19. Using data from patients from South India, Saathvik Kannan, a senior at Hickman High School and a computer programmer and researcher for the Singh lab, tracked changes to the virus’ proteins.
“Viruses are known to evolve under pressure, so what’s happening in this case is that antibodies recognize the virus in a cell, and the virus sees that, ‘okay, there is someone to stop me,’ so it makes mutations,” Sing said.
The virus’ genome often alters, by mutating, inserting, or deleting the building blocks within RNA and DNA known as nucleotides, depending upon the pressure that viruses experience. Only some of these sugar-containing nucleotides are mutated, but these small changes can form a new virus variant.
“A few months ago, we didn’t know the reason behind all of these different mutations in patients because we did not look for APOBEC-mediated changes in viral genome,” Singh said.
Kannan found that between October 2022 to January 2023, the mutations among the patient cohort varied between 114 to 83. With that information, he identified 50% of patients who have diabetes and that when they take insulin the APOBEC protein is also induced. This new discovery leads to more questions about those with underlying conditions like diabetes or hypertension, and how they are affected differently by the drug.
“Ideally if a virus were to evolve you would see a linear progression, but you don’t see that here,” Kannan said. “This shows us that APOBEC proteins are likely one of the causes of this evolution in the virus and the makers of these variants.”
When the number of mutations vary significantly, like in the cohort, it re-affirms that the COVID-19 variants evolve independently.
Viruses don’t stop to wait for researchers to find the root of the problem. They constantly change, and in cases where the patients are vaccinated and take remdesivir, the virus evolves by taking advantage of the APOBEC protein.
Singh started down this path of research early on in the pandemic. Through PCR tests — which converts tiny amounts of RNA into DNA then copies it to a measurable level — he learned more about each mutation by comparing new samples to the original viral strain. Until this point, there had only been around 40 identified mutations in the spike protein in the different XBB sub-variant, but Singh’s lab has identified two more. The details have been recently published in The Lancet Journal. The two mutations found in this process, A27S and T747I, were unique to this cohort.
“For the first time we’re able to get more clues on what is actually happening because we were able to compare it to patient samples in the XBB subvariant and we had a wealth of data to work with,” Kannan said.
The Omicron variant yields new mutations constantly — currently at 43 and counting — and presents plenty of opportunity to look for differences. Singh directs his team to comb through variant sequences to identify differences in their genetic code. Soon they begin to identify trends from one month to another.
“The main difference here was that we have high quality patient data this time, from a patient cohort in Southern India, as opposed to getting it from a database,” Singh said. “The patient cohort tells us that the mutations are more than what was reported before.”
From January to June of 2020, Kannan found mutations that were present in one hundred percent of the sequences. When the Alpha Beta variant arrived in November 2020, they immediately knew what the mutated changes were. Their findings were published in the paper, ‘Clinical characteristics and novel mutations of omicron subvariant XBB in Tamil Nadu, India – a cohort study,’ in April 2023 in the Lancet Regional Health – Southeast Asia Journal.
After new variants — such as the XBB sub-variant of Omicron — materialized, Singh’s lab identified existing drugs and new drug compounds that match structural weaknesses presented by mutations.
One way Singh’s lab keeps abreast of new variants is by utilizing the tools they have available to their advantage with in-house programs either in Python or in R programming languages. Their lab can construct non-infectious, virus-like particles that contain all the same characteristics as the virus minus its genome, or its genetic material makeup.
A collaboration between University of Missouri and University of Nebraska Medical Center helped identify the new drug compound, MU-UNMC-2 in addition to the MU-UNMC-1, previously found in late 2021, as potential coronavirus treatments.

Remdesivir, ribavirin, favipiravir, and molnupiravir were among existing drugs that can be used to treat COVID-19 under certain conditions. Remdesivir — previously ineffective as an Ebola virus treatment — initially proved somewhat useful for COVID-19. Molnupavir only showed moderate promise, and the two drugs were approved for emergency use by the FDA for the treatment of COVID-19. Remdesivir now has full FDA approval.
“To address the problem, you have to find the problem. Where is the virus? What can we address? And then we go after it,” Singh said. “My lab was the first one in the world who suggested when the pandemic came that these are a few drugs that can be used and remdesivir was one of them. I’m very proud that I could contribute to human health in that way.”
With knowledge of this new protein in hand, Singh’s lab now is moving forward to focus most of their attention on the APOBEC protein mediated mutations and how underlying health conditions can affect an individual’s reaction to certain drug compounds.
“The virus has been outsmarting us, outfoxing us, until now. As soon as we get something, it changes itself,” Singh said. “That keeps us motivated as we chase it.”
The Singh lab’s research on the XBB sub-variant mutations was published in the paper ‘Omicron SARS-CoV-2 variant: Unique features and their impact on pre-existing anitbodies’ in the “Computational and Structural Biotechnology Journal” in June 2021 and their updated findings can be found in the paper ‘Clinical characteristics and novel mutations of omicron subvariant XBB in Tamil Nadu, India – a cohort study,’ published in “The Lancet Regional Health – Southeast Asia Journal” in April 2023.
Funding provided by: Bond LSC, Swedish research Council, American Lung Association, National Institute of Dental and Craniofacial Research in collaboration with Prof. Gary Weisman of the Bond Life Sciences center.

