Bond LSC lab reveals how a missing iron protein can cause muscle weakness
By Roger Meissen | Bond LSC
Aging brings muscle weakness seen in the lack of strength of a handshake or the sureness of movement.
That atrophy is no accident, and it traces back to how cells, particularly their energy-producing components, decline in function as we climb in years.
One University of Missouri researcher’s latest discovery, published this week in Proceedings of the National Academy of Sciences, shows a distinct cellular reason why this weakness occurs.
His lab revealed how a muscle cell’s mitochondria fail to generate enough energy for skeletal muscles due to one iron–sulfur protein. This understanding could one day help lead to treatments for diseases like Duchenne muscular dystrophy — the most common type of muscular dystrophy in children — and muscle deterioration associated with aging.
“We followed the phenotype, the muscle weakness in our mice, to this protein,” said Ron Mittler, a principal investigator at Mizzou’s Bond Life Sciences Center and a plant biologist. “What we found is that CISD3 proteins — also found in our bodies — are important for regulating the levels of iron in the mitochondria, and previously nobody knew what they were doing.”
The importance of a single protein
CISD3 — (conserved iron-sulfur domain-containing protein 3) — exists solely inside a cell’s mitochondria, the organelle responsible for creating the energy for the cell. To figure out its function, the Mittler lab started by disabling the genetic code for it in test mice. Lab manager, Linda Rowland, noticed a particular lack of strength in these knockout mice compared to normal mice. Lab members confirmed the knockout mice were weaker through physical observation and strength measurements then used a series of tests to prove why. By analyzing the proteins in the model mouse and studying the structure of them, they found a markedly lower concentration of the CISD3 protein.
“Mitochondria in muscles are highly energetically active, but we found they were in very bad shape in these knockout mice,” Mittler said. “After that, we completed proteomic and structural studies, because we wanted to see what this CISD3 protein actually does.”
In this process, they noted that the reduced CISD3 binds closely with several proteins in respiratory chain complex I and II and transfers one of its iron clusters for its metabolic process. Without this chemical binding and transfer, some important cell respiration processes within the mitochondria don’t happen, reducing how much food is converted into an energy form that cells can use.
“Basically, complex I is almost shut down completely in the knockout mice, and that’s why they have weak muscle and die earlier,” Mittler said.
To confirm this interaction, Mittler’s lab partnered with scientists at Rice University and University of Texas to compare CISD3 protein with proteins from the respiratory complex one. The computational biology approach analyzes how proteins may have evolved together. When two proteins interact, scientists see fewer mutations over time. Using AI models, they predicted and ranked the likelihood of protein-to-protein interaction. They saw almost no mutations between these proteins, confirming that CISD3 binds with the NDUFV2 protein of the respiratory complex I.
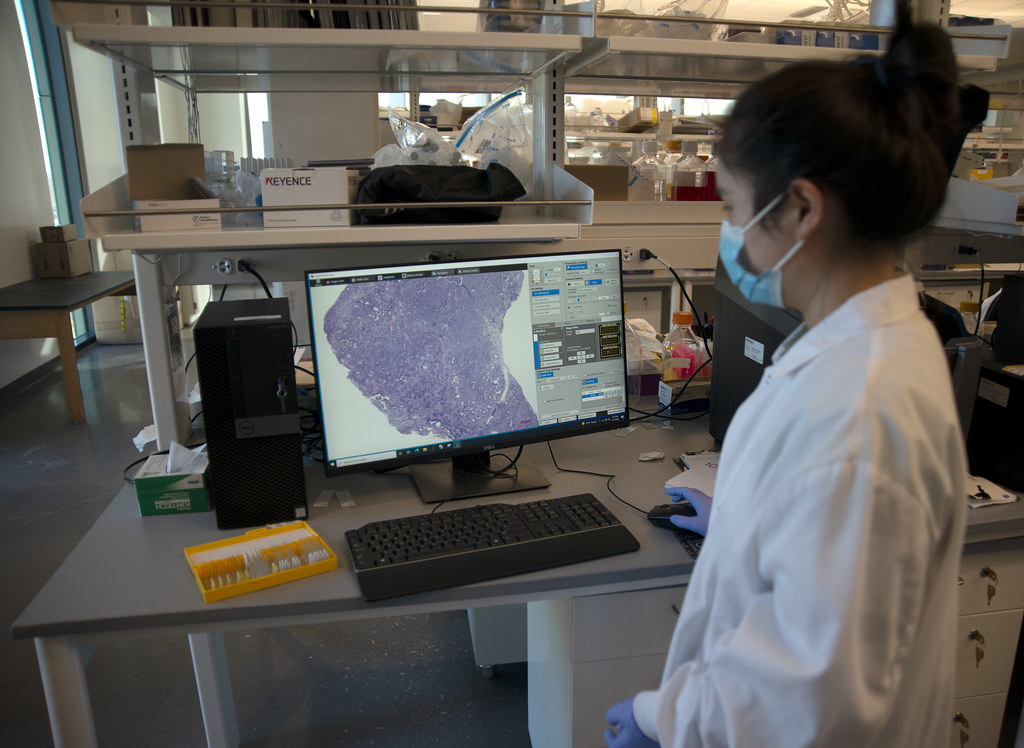
Finally, the researchers utilized equipment at the Roy Blunt Precision Medicine building to further examine the metabolic function in skeletal muscle cells. Using Seahorse analyzers and muscle fibers they generated, they measured the rate of respiration, glycolysis and many other processes. With the knockout mouse muscle cells missing CISD3, they saw very little respiration and elevated glycolysis — where sugars are broken down into energy without needing oxygen like in respiration.
From plants and cancer to muscles
It’s been a long interaction between Mittler and iron-sulfur proteins.
He first happened upon this protein family in 2007 after he received a National Science Foundation grant to study proteins of unknown function. As a plant biologist, he detailed how CISD1 made model plants more resistant to oxidative stress when overexpressed. Oxidative stress is detrimental to cells because of increased levels of reactive oxygen species that make cells deteriorate faster.
“The plants actually looked bigger, they were happier,” Mittler said. “We initially didn’t know anything about this plant protein, and when we found the same protein in mammals, we then asked where that protein was important in animals.”
That question led him to study cancer where his team found lots of these iron-sulfur proteins, and when Mittler moved to the University of Texas in 2010, he shifted to also understand the protein in animals.
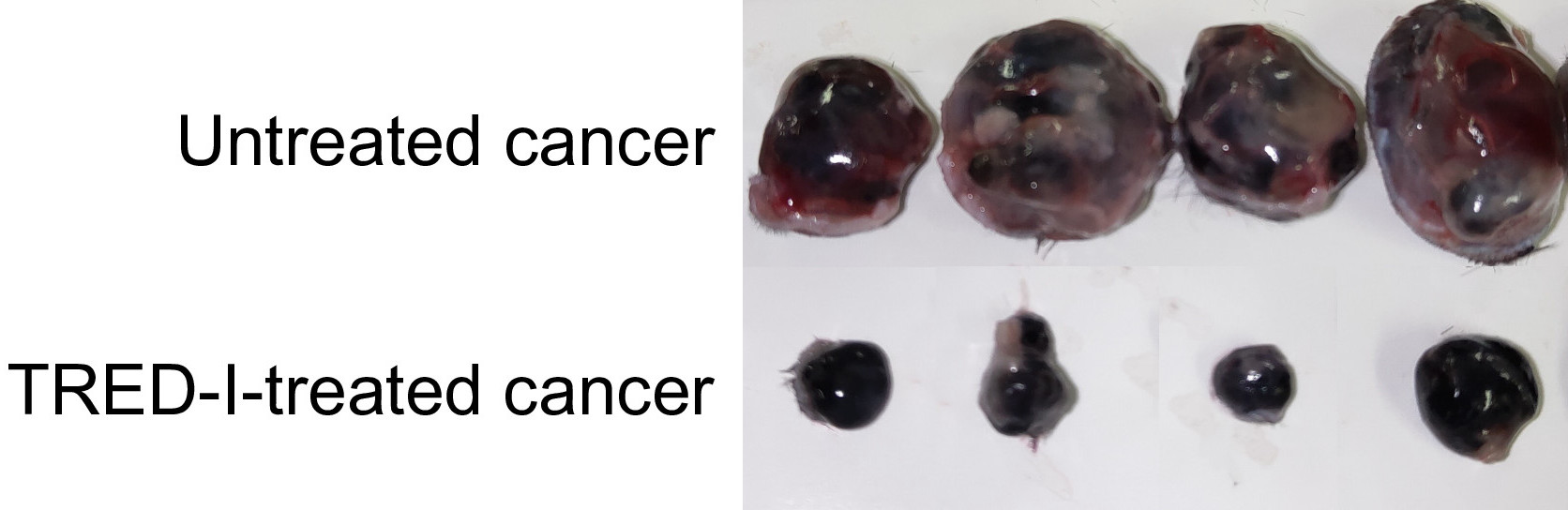
“Cancers like breast cancer are known to have what scientists consider an ‘iron addiction’ and thrive on having a lot of it, therefore they need a lot of all three of these proteins,” he said. “If you want a lot of cell proliferation, like in cancers, you need a lot of these iron clusters and reactive oxygen.”
This current study is his first foray into normal development instead of disease and destruction.
Moving research from lab to startup
Regardless of species, all this knowledge of sulfur-iron proteins has given Mittler the information and experience to pursue applications.
“For this study, there are a lot of applications from the standpoint to developing drug therapies for disorders such as Duchenne’s Muscular Dystrophy, or for CISD3, it’s possible to develop a genetic screen for embryos that doesn’t have respiratory complex I working,” he said.
He recently founded a startup company called MitoMed to develop drugs based on these sulfur-iron proteins.
“I’m trying to develop drugs to fight cancer because I think, for us, this is what will make a big difference,” he said. “We already have one type of drug with almost no side effects; we’ve done all the mouse work and the idea now is to get this to clinical trials.”
The paper “CISD3/MiNT is required for complex I function, mitochondrial integrity, and skeletal muscle maintenance” published in Proceedings of the National Academy of Sciences on May 23, 2024. Collaborators from the University of Missouri, Rice University and the University of Texas worked on this paper. This work was partially supported by grants from the National Institutes of Health, the National Science Foundation and the U.S.-Israel Binational Science Foundation.