By Becca Wolf | Bond LSC
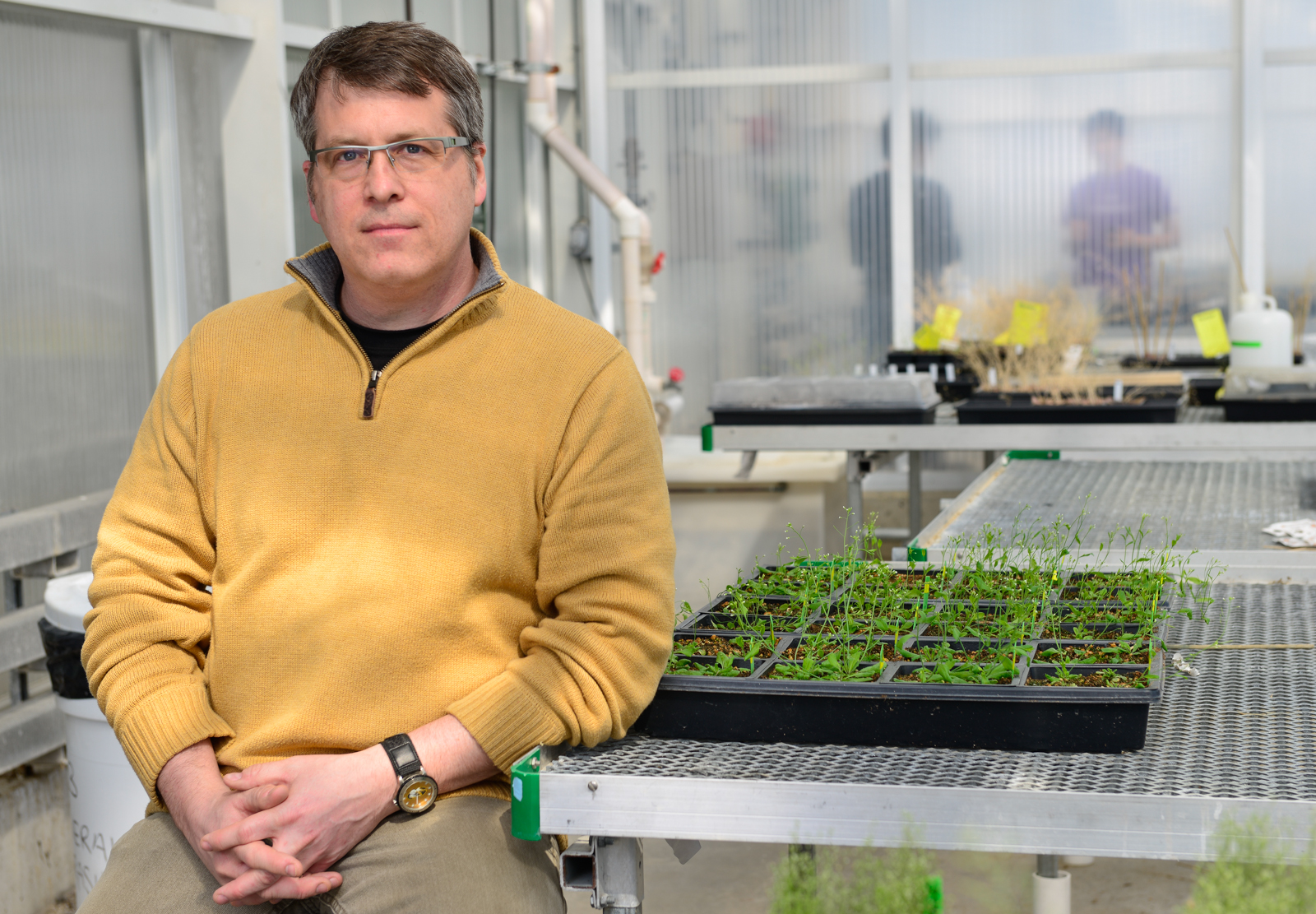
Medical bacteriologist, George Stewart has had a few stops along the way before he got to Bond LSC in 2004. Having done schooling and research at universities from the midwest to the east coast, it has been a long journey filled with many ups and downs, but a rewarding one at that.
Stewart hadn’t always wanted to be a medical bacteriologist though, “When I was going to college, I actually wanted to be a marine biologist,” he says, “And then my sophomore year in college, I took a microbiology course. And that changed that.”
This microbiology course at the University of North Texas was the first course where he was able to do hands on work in a laboratory and he found that, “culturing organisms and identifying organisms was very appealing.”
“The technological advancements are so fast in this discipline that you just have to change and there are easier ways to do things and better ways to do things now,” he states.
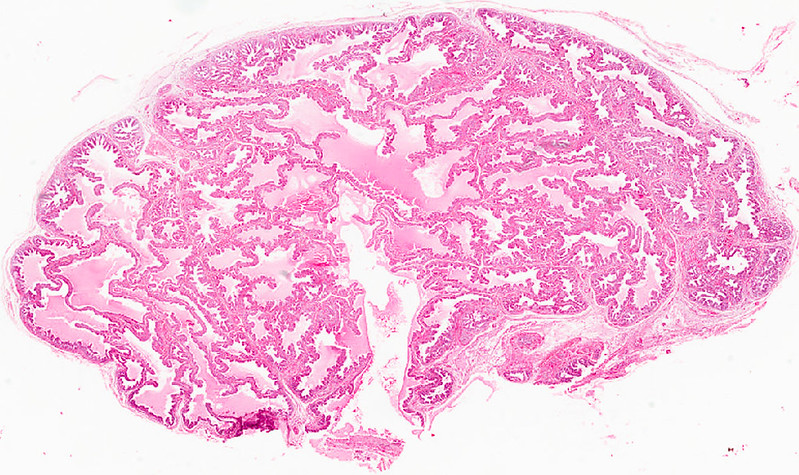
But these changes help Stewart delve deeper in understanding his passion for an organism best known for the white powder derived from its spores and sometimes used in terror attacks. Technically called Bacillus anthracis, the organism causes the disease anthrax. Stewart focuses on the outer spore of the bacteria which first comes in contact with the infected host and is responsible for protein production. He looks at how the spore contributes to anthrax’s ability to persist in soil and how it contributes to resistance properties.
Unfortunately for Stewart, funding for anthrax research has declined over the years, “It’s not considered a high priority organism,” he explains, however, “it still is an organism of concern for bio-threats.” To work around the lack of funding, Stewart has turned in other directions.
“Part of that has actually been the biggest success stories of recent times in my lab,” he said.
The direction? Using Bacillus thuringiensis, a bacterium similar to anthrax, to do research on. One problem Stewart approached using this bacterium was cleaning up Atrazine, a herbicide used by farmers to kill weeds. This herbicide, while helpful to farmers, can contaminate groundwater, potentially causing diseases in humans.
To find a solution, Stewart and Brian Thompson, a postdoc student in his lab, collaborated with Chung-ho Lin, a research associate professor in the MU Center for Agroforestry, “looking at could we possibly have come up with approaches using this basic technology to improve agriculture from a number of different ways to make plants grow faster, better, that sort of thing.”
They found that they could display proteins on Bacillus thuringiensis spore that would break down Atrazine. Farmers would only have to spray their fields with this organism and the soil would be clean of Atrazine.
Taking this a step further, Thompson created the company, Elemental Enzymes, to sell products like this to farmers in order to clean the environment. Located in St. Louis, Elemental Enzymes currently has 11 products in use today on more than 11% of corn acres in the United States in 2019, and that number seems to be increasing.
“It’s kind of interesting in the sense that we started off trying to answer a very basic biological question related to spore biology and involving a significant high consequence pathogen, and we ended up discovering something which has huge benefits for agriculture. So you never know what direction it’s going to take you in these things,” says Stewart.
Stewart hasn’t stopped there. In fact, he was one of the driving forces behind starting a Bachelor of Science degree program in microbiology here at MU. After a microbiology degree program here was discontinued in the early 2000s, Stewart has since found evidence that the degree would be successful here at the university and it was approved by the board of curators and the Missouri Department of Higher Education in 2018. The first students in this program began this past semester and Stewart says, “we’re getting underway.”
Despite these accomplishments, Stewart is getting ready to retire this year, explaining, “part of the reason that I stayed on this year was to make sure this program gets off the ground and help out with that.” While his career is winding down here at MU, he is still keeping busy, “I’m actually teaching two undergraduate courses in microbiology, once called fundamentals of microbiology, it’s an introductory microbiology course. And the other one is public health microbiology, which is more of a junior level type course.”
He also continues to do some work in his lab as he has two graduate students finishing up their degrees this year and recently stepped down as the Department of Veterinary Pathobiology chair in January.
What does Stewart have planned for when he retires? He is not slowing down, that is for sure. Stewart and his wife already have a vacation planned for New Zealand within the next few months, and he plans on spending quality time with his children and grandchildren.
“I won’t have accomplished all the things I wanted to,” he says, “but I think we’ll have gotten the major things done. So that’s satisfying.”