Imagine researchers in hazmat suits moving slowly and deliberately through a lab. One of them holds up a beaker. It’s glowing.
This light — or the absence of it — could save millions of dollars for governments and save the lives of anthrax victims.
Scientists at the University of Missouri Laboratory of Infectious Disease Research proved a new method for anthrax detection can identify anthrax quicker than any existing approach.
When the “bioluminescent reporter phage” — an engineered virus — infects anthrax bacteria, it takes on a sci-fi-movie-type glow.
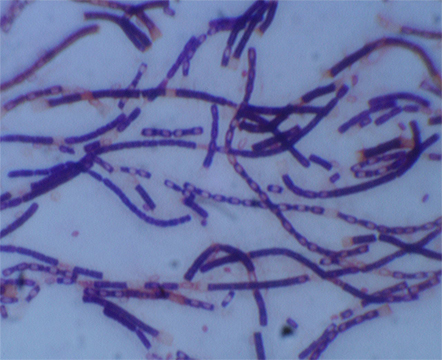
George Stewart, a medical bacteriologist at MU’s Bond Life Sciences Center, and graduate student Krista Spreng, observed the virus against a variety of virulent strains of bacillus anthracis, the bacteria causing anthrax disease.
“For this technique, within a few hours, you’ll have a yes or no answer,” Stewart said.
The research, funded by the USDA, was published in the Journal of Microbiological Methods in Aug. 2013. David Schofield at Guild BioSciences, a biotech company in Charleston, S.C, created the reporter phage.
This new method could save a significant amount of money associated with the decontamination of anthrax from suspected infected areas.
Expensive clean-up from the 2001 “Letter attacks”
With the country on high-alert following Sept. 11, 2001, a slew of bioterrorists mailed anthrax letters, filled with a powder that if inhaled could cause death.
Numerous Post Offices and processing facilities were closed and quarantined.
The clean-up bill for the 2001 Anthrax Letter attacks was $3.2 million, according to a 2012 report in Biosecurity and Bioterrorism: Biodefense Strategy, Practice and Science.
Theoretically, the new detection method would alert of a negative result potentially five hours into clean-up efforts instead of two or three days into expensive decontaminating.
Current methods take anywhere from 24 hours or longer to produce a definitive answer for anthrax contamination.
A five-hour benchmark
Stewart said from contamination levels expected from a bioterrorism threat, a positive answer could be found in five hours. If contamination levels were higher, results would come back much more quickly.
Prior to this bioluminescent reporting phage, experts used techniques that were culture based or PCR (polymerase chain reaction) based. Both methods, require additional time for a definitive answer, a minimum of 24 to 48 hours, Stewart said.
“Normally to identify whether an organisms is present, you have to take the material culture, the organism and all the bacteria that might be present in the sample,” Stewart said. “You have to pick colonies that might be bacillus anthracis and do chemical testing which takes some time.”
From a bio-threat standpoint, breathing in anthrax, is the highest concern for public health and homeland security officials and has the highest fatality rate among forms of anthrax.
“If you have a situation and need a quick yes or no answer, this is a tool that will help that,” Stewart said.
Terrorists have used a powder form of anthrax, which has been slipped into letters of political persons and media. A person is infected when an anthrax spore gets into the blood system, most commonly through inhalation or an abrasion on the body, according to Centers of Disease Control and Prevention.
For low levels of contamination, the bioluminescent reporter phage would still detect the presence of the bacteria, but it would take longer.
“This method will be as quick as any of the others and quicker than most,” Stewart said.
The bioluminescent-detection method can detect low levels of anthrax bacteria and rule out false positives. The added benefit to this reporting system is its ability to show that anthrax bacteria are present and it’s alive, Stewart said.
What’s next?
The next step in the bioluminescent reporter phage is getting it approved so a product can be produced and branded. The agency that would warrant the stamp of approval would depend on the eventual use of the phage — food-related testing would likely go through the Food and Drug Administration, Stewart said.
When that happens, a product would not necessarily require a formal lab — it would need a place where cultures could grow at 37 degrees.
“Samples could be collected, brought back to the state public health lab for example and then the testing could be done within a few hours of the collection of the samples and you would have a result,” Stewart said.
The last anthrax attack was in 2001, but the possibility of one happening again, Stewart said, remains a driver for proactive research.
“In the years since the postal attacks, we haven’t had any bona fide anthrax attacks,” Stewart said. “That doesn’t mean it’s not going to happen — we have to be prepared for when it does occur again.”
Stewart’s research on anthrax bacteria and detection methods recently appeared in the August 2013 edition of The Journal of Microbiological Methods.

